Expression of aquaporin channels 1 and 5 during mechanical ventilation
2010, European Journal of Anaesthesiology
https://doi.org/10.1097/00003643-201006121-00296…
305 pages
1 file

Sign up for access to the world's latest research
Abstract
AI
AI
This study investigates the expression of aquaporin channels 1 and 5 during mechanical ventilation, focusing on their roles in fluid homeostasis and cellular responses in the lungs. The research highlights changes in the levels of these channels under various mechanical ventilation settings, contributing to our understanding of ventilatory impact on pulmonary function and the potential for targeting aquaporins in therapeutic strategies.



















![Materials and Methods: After suffering two cases of possible reactions in operating room. We review what has been done retrospectively and the it- erature, we found gaps in the diagnostic phase that generated an increase in avoidable costs, so we set contact the Allergy Service of our hospital, result of this collaboration is this article and following algorithm. Results and Discussion: As a guideline the Community of Castilla la Mancha sets prices for specialized medical tests, diagnosis and treatment in the first consultation by 185.22 euros and 69.42 euros in successives. [8]. These patients have an average of three consultations of allergy to the final diagnosis. If we stick to our hospital surgical activity in 2005: 44.367 events, applying the percentages of the introduction there would be 3 “true” allergic reactions which require monitoring by the Department of Allergy and 30 cases of anaphylactoid reaction in which an initial determination of tryptase would have saved 9721.8 euros to the hospital.](https://figures.academia-assets.com/48316896/figure_011.jpg)




























![Values are expressed as number of patients (%). CRO: complete response(CR) of PACU 1 min, CR1: CR of postoperative 1hr CR2: CR of postoperative 2hr CR6: CR of postoperative 6hr CR24: CR of POD 1 CR48: CR of POD 2, No vomiting 24: no vomiting 0-24h after surgery, tP < 0.05, compared with control group. [table2]Percent of complete response and proportion of no vomiting](https://figures.academia-assets.com/48316896/table_028.jpg)

















































![aN Se a a ee ee EE ee aS ae ee and were randomly assigned to receive either balanced xenon or sevoflurane anaesthe- sia with remifentanil titrated to clinical needs. BIS monitoring was blinded to the perform- ing anaesthetist and values were continuously assessed by accessory study personnel. Results and Discussion: 30 patients were enrolled in each group, comparable in respect to age, gender, height, ASA status, baseline systolic blood pressure anc baseline heart rate. BIS values during induction and maintenance of xenon anaesthe- sia correlated well with the value range recommended for deep hypnosis and with val- ues obtained during sevoflurane anaesthesia.Bispectral Index monitoring thoroughly indicated an adequate level of hypnosis during balanced xenon anaesthesia guidec according to clinical parameters. Controversial results obtained from former studies [2] indicating unpredictable influences of xenon on the BIS were not confirmed.](https://figures.academia-assets.com/48316896/figure_051.jpg)







![Daca cts Figure 2. Steady-state detection results for one patient outside the training set. From top to bottom: drug's effect-site concentration targets and arithmetic rule DIF; filtered BIS, filtered mean blood pressure and filtered ECG heart rate with the input steady-state periods overlapping; combined measure of output steady-state. Results and Discussion: 22 patients, 12 men, 55.9+13.0 years, 69.3413.4kg and 164.346.9cm. Fig. 2 presents the results for one patient outside the training set, with the inputs SS detection followed by the filtered signals (BIS, ECG heart rate and blood pressure) and combined measure of SS. The performance of the method was visually evaluated, with the results indicating an adequate detection of the SS periods. We also observe that SS in the inputs is not always followed by SS in the output signal [4], this may be the result of external interferences not only related to the input drugs.](https://figures.academia-assets.com/48316896/figure_056.jpg)
![Figure 1. Diagram presenting the algorithm steps: the patient is the system, with propofol and remifentanil drugs effect-site concentrations (Cc) as inputs, and mean blood pressure (MBP), ECG heart rate (HR) and BIS as measurable outputs. On top we have the steady- state detection arithmetic rule for the inputs, and on bottom we have the wavelet based algorithm summary to determine the combined steady-state index. Materials and Methods: Data collected every 5 s (Rugloopll) during 22 urologi- cal procedures under TCI of propofol and remifentanil (Gchnider [1] and Minto’s [2] PkPd models). Data from 5 patients used to extract periods of SS by visual analysis, and tuning parameters for the wavelet detector [4]. The tuned algorithm was applied to all patients. Drugs SS periods were identified by an arithmetic rule. Fig. 1 summa- rizes the algorithm. The SS index varies from O (non-SS) to 1 (SS), with smoothing period of 15s. MATLAB R2007a was used for signal analysis.(Data: Mean+SD)](https://figures.academia-assets.com/48316896/figure_057.jpg)





















![Figure2. Kaplan-Meier Survival Analysis of Patients with normal and elevated Postoperative Troponin I. Results and Discussion: Findings: Of 378 patients, who underwent major head and neck cancer surgery, 57 patients (15%) developed an elevated Tnl; 90% of which occurred within the first 24 hours after surgery. Pre-existing renal insufficiency (unadjusted OR [OR]: 4.60, 95% Cl 1.53-13.82), coronary artery disease (OR: 2.33, 95% Cl 1.21-4.50), peripheral vascular disease (OR: 2.83, 95%Cl 1.31-6.14), hypertension (OR: 2.22, 95% Cl 1.20-4.12), and previous combined chemotherapy and radiation (OR: 2.68, 95% Cl 1.04-6.91) were asso- ciated with elevated postoperative TnI. Patients with elevated Tnl had a signifi- cantly longer length of stay in the hospital (8.5 vs. 10.1 days; p= 0.014) and ICU (8 vs. 4.5 days; p= 0.001) and an 8-fold increased risk of death at 60 days after surgery (OR 7.62; 95% Cl 1.98 — 29.31). At one year, patients with an abnormal postoperative Tnl were twice as likely to die (OR 1.93; 95% Cl 1.02 — 3.63).](https://figures.academia-assets.com/48316896/figure_071.jpg)



















![Respiratory parameters during both periods (n=82) Conclusion(s): During OLV, PEP does not maintain oxygenation when V, is reduced. Lowering Vt might be efficient in reducing lung injury but the use o' such protocol may require the acceptance of possibly lower PaO, and alveolar ventilation. Results and Discussion: ]V, = tidal volume, RR = respiratory rate, Pplateau = end inspiratory plateau pressure, PEEP = positive end expiratory pressure, Pmean = mean alveolar pressure, Pe,CO, = end tidal CO,, PaCO, = arterial carbon dioxide tension, PaO, = arterial oxygen tension, SAP=Systolic arterial pressure. HR = Hear Rate. The PaO,/FiO, ratio significantly decreased during low Vt ventilation (mean difference = -18.8; 95% IC [-34.0 to -3.5], P=0.02). Any significant increase of intrinsic PEEP has been observed between both groups.](https://figures.academia-assets.com/48316896/table_072.jpg)

















































![Figure Arteriovenous fistula occlusion rates 6-weeks and 3-months after surgery. Data expressed as percentage of patients GA, general anesthesia, RA, regional anesthesia, LA, local anesthesia GA, general anesthesia; RA, regional anesthesia; LA, local anesthesia; LOS, length of stay. Data expressed either as mean + SD, median [range], or number of patients (%).](https://figures.academia-assets.com/48316896/figure_104.jpg)







































![Data = https://www.academia.edu/28010776/effect site concentrations of Propofol (mean + SD (ug/ml); * P<0.05 as compared to saline Table 1. Effect of Clonidine on Propofol requirements haemodynamics were aicilar in both groups. Effect site concentrations of PROP [table 1] and REMI [table 2] were significantly less in clonidine group (respectively P=0.029 et P=0.05).](https://figures.academia-assets.com/48316896/table_119.jpg)





















![Results and Discussion: Six patients were identified,all of whom had some form of neuraxial blockade. Table 2 shows the risk factors for each patient. [table1]Many of these risk factors relate to being in labour itself but when com- bined with neuraxial blockade,surgery or a critical care stay,parturients are at high risk of developing pressure ulcers.](https://figures.academia-assets.com/48316896/table_135.jpg)









![Results [All data presented as median (lQR)]](https://figures.academia-assets.com/48316896/table_141.jpg)
















































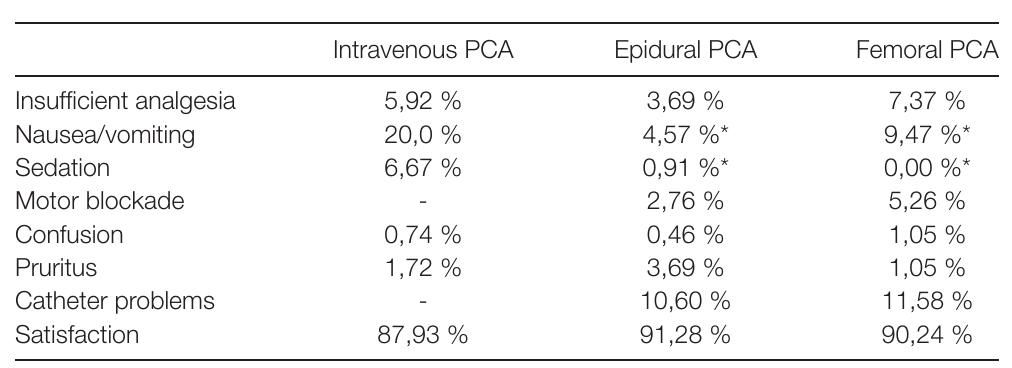
![Results and Discussion: 135 patients received in the postoperative period intravenous patient-controlled analgesia (PCA) with morfine, 217 epidural PCA and 95 femoral nerve PCA. Following pain scores (numeric rating scale) were observed: Following complications, adverse effects and patient satisfaction were observed:[table2]Patients with epidural and femoral nerve PCA had lower pain scores on movement 24 and 48 hours postoperatively and less nausea/ vomiting and sedation than patients with intravenous PCA with morfine.](https://figures.academia-assets.com/48316896/table_166.jpg)






















![Conclusion(s): Performance of electrostatic filters in the clinical setting may not be worse than pleated filters. Factors other than patient contamination levels Results and Discussion: 8/86 (9%) filters had excessive contamination on the machine side. However, only one of these was also contaminated on the patient side. Previous studies have mainly shown contamination on the machine side if it also occurred on the patient side. Lower levels of contamination on the machine side were observed in the current study compared to previous testing of electrostatic filters (9% versus 13%) [ref 2]. However, previous data for electrostatic filters was from a paediatric population where patient side con- tamination levels were higher. There did not appear to be a significant difference in ‘failure rate’ between the small electrostatic filter in this study and a pleated filter in a previous study (8% vs 9%) [ref 2].](https://figures.academia-assets.com/48316896/table_179.jpg)












![Conclusion(s): EVA proved to be efficient in restoring oxygenation quickly and limiting hypercarbia over a period of 15 minutes through a 2 mm transtracheal catheter in hypoxic pigs with a completely obstructed upper airway. Results and Discussion: The minute volume necessary to maintain nor- moventilation during IPPV was 9.9 [9.1-12.0] L/min. After 2 minutes of apnea EVA restored oxygenation within 10 seconds.](https://figures.academia-assets.com/48316896/table_183.jpg)




![*responders chose one or more options. Conclusion(s): The findings of this survey suggest that the majority of units use DLT as the method of lung isolation. This may be related to the well docu- mented advantages of DLT over BB [1]. Our findings suggest that gender and height are most likely to be used to predict DLT size. Although the CXR tracheal diameter is more predictive [2], it was the least used criteria. When managing an unpredicted difficult airway, 73% of units used tracheal tube introducer to guide DLT insertion. Caution is advised when this technique is used as the Frova, cur- rent gold standard single-use introducer, is not recommended for use with DLT. When confirming DLT position, 7.7% of units use clinical examination, 19.2% of units use fibreoptic scope and 73% of the units use both methods. Fibreoptic confirmation is recommended given the anatomical variations in the tracheo- bronchial tree and the adverse complications of a misplaced DLT. Dafavenmnnanc:](https://figures.academia-assets.com/48316896/table_186.jpg)












![VATS, video-assisted thoracoscopy; (n), number of patients Materials and Methods: We selected 22 ASA I-Il patients (without predicted difficult airway management and with normal pulmonary function tests [FVC> 80% and FEV1 > 80% predicted]) undergoing different thoracic surgery proce- dures in which one lug ventilation was necessary. Lung isolation was achieved introducing the bronquial blocker through the I|-GEL supraglottic device under direct flexible fibrobroncoscopic vision.](https://figures.academia-assets.com/48316896/table_195.jpg)




![Abstract 19AP6-1 — Impulse, Peak Force and Time to Intubation with GVL in Four Manikins Data expressed as median [IQR], N=Newton, s=seconc](https://figures.academia-assets.com/48316896/table_197.jpg)








![Data expressed as median [IQR]. Impulse (Newtons/second). Peak Force (Newtons). A=Laerdal®SimMan, B=Trucorp AirSim™™Advance, C=Laerdal@Airway Management Trainer, D=Ambu®Airway Man. Impulse and Peak Force with MDL and GVL](https://figures.academia-assets.com/48316896/table_202.jpg)





























Key takeaways
AI
AI
- The study assesses the expression of aquaporin channels 1 and 5 during mechanical ventilation.
- Inflammatory markers and memory performance were evaluated post-surgery and LPS administration.
- Propofol pharmacokinetics in infants shows significant clearance differences based on age.
- Intraoperative 'Triple Low' conditions predict poor postoperative outcomes.
- A standardized postoperative care protocol improved outcomes and reduced complications.
Related papers
British Journal of Anaesthesia, 2005
After alarming reports concerning deaths after sedation with propofol, infusion of this drug was contraindicated by the US Food and Drug Administration in children &lt;18 yr receiving intensive care. We describe our experiences with propofol 6%, a new formula, during postoperative sedation in non-ventilated children following craniofacial surgery. In a prospective cohort study, children admitted to the paediatric surgical intensive care unit following major craniofacial surgery were randomly allocated to sedation with propofol 6% or midazolam, if judged necessary on the basis of a COMFORT behaviour score. Exclusion criteria were respiratory infection, allergy for proteins, propofol or midazolam, hypertriglyceridaemia, familial hypercholesterolaemia or epilepsy. We assessed the safety of propofol 6% with triglycerides (TG) and creatine phosphokinase (CPK) levels, blood gases and physiological parameters. Efficacy was assessed using the COMFORT behaviour scale, Visual Analogue Scale and Bispectral Index monitor. Twenty-two children were treated with propofol 6%, 23 were treated with midazolam and 10 other children did not need sedation. The median age was 10 (IQR 3-17) months in all groups. Median duration of infusion was 11 (range 6-18) h for propofol 6% and 14 (range 5-17) h for midazolam. TG levels remained normal and no metabolic acidosis or adverse events were observed during propofol or midazolam infusion. Four patients had increased CPK levels. We did not encounter any problems using propofol 6% as a sedative in children with a median age of 10 (IQR 3-17) months, with dosages &lt;4 mg kg(-1) h(-1) during a median period of 11 (range 6-18) h.
British Journal of Anaesthesia, 2007
Background. Propofol is commonly used in children undergoing diagnostic interventions under anaesthesia or deep sedation. Because hypoxaemia is the most common cause of critical deterioration during anaesthesia and sedation, improved understanding of the effects of anaesthetics on pulmonary function is essential. The aim of this study was to determine the effect of different levels of propofol anaesthesia on functional residual capacity (FRC) and ventilation distribution. Methods. In 20 children without cardiopulmonary disease mean age (SD) 49.75 (13.3) months and mean weight (SD) 17.5 (3.9) kg, anaesthesia was induced by a bolus of i.v. propofol 2 mg kg 21 followed by an infusion of propofol 120 mg kg 21 min 21 (level I). Then, a bolus of propofol 1 mg kg 21 was given followed by a propofol infusion at 240 mg kg 21 min 21 (level II). FRC and lung clearance index (LCI) were calculated at each level of anaesthesia using multibreath analysis. Results. The FRC mean (SD) decreased from 20.7 (3.3) ml kg 21 at anaesthesia level I to 17.7 (3.9) ml kg 21 at level II (P,0.0001). At the same time, mean (SD) LCI increased from 10.4 (1.1) to 11.9 (2.2) (P¼0.0038), whereas bispectral index score values decreased from mean (SD) 57.5 (7.2) to 35.5 (5.9) (P,0.0001). Conclusions. Propofol elicited a deeper level of anaesthesia that led to a significant decrease of the FRC whereas at the same time the LCI, an index for ventilation distribution, increased indicating an increased vulnerability to hypoxaemia.
Frontiers in immunology, 2017
Aside from direct effects on neurotransmission, inhaled and intravenous anesthetics have immunomodulatory properties. In vitro and mouse model studies suggest that propofol inhibits, while isoflurane increases, neuroinflammation. If these findings translate to humans, they could be clinically important since neuroinflammation has detrimental effects on neurocognitive function in numerous disease states. To examine whether propofol and isoflurane differentially modulate neuroinflammation in humans, cytokines were measured in a secondary analysis of cerebrospinal fluid (CSF) samples from patients prospectively randomized to receive anesthetic maintenance with propofol vs. isoflurane (registered with http://www.clinicaltrials.gov, identifier NCT01640275). We measured CSF levels of EGF, eotaxin, G-CSF, GM-CSF, IFN-α2, IL-1RA, IL-6, IL-7, IL-8, IL-10, IP-10, MCP-1, MIP-1α, MIP-1β, and TNF-α before and 24 h after intracranial surgery in these study patients. After Bonferroni correction fo...
Anesthesiology, 2006
Background To support safe and effective use of propofol in nonventilated children after major surgery, a model for propofol pharmacokinetics and pharmacodynamics is described. Methods After craniofacial surgery, 22 of the 44 evaluated infants (aged 3-17 months) in the pediatric intensive care unit received propofol (2-4 mg . kg-1 . h-1) during a median of 12.5 h, based on the COMFORT-Behavior score. COMFORT-Behavior scores and Bispectral Index values were recorded simultaneously. Population pharmacokinetic and pharmacodynamic modeling was performed using NONMEM V (GloboMax LLC, Hanover, MD). Results In the two-compartment model, body weight (median, 8.9 kg) was a significant covariate. Typical values were Cl = 0.70 . (BW/8.9)0.61 l/min, Vc = 18.8 l, Q = 0.35 l/min, and Vss = 146 l. In infants who received no sedative, depth of sedation was a function of baseline, postanesthesia effect (Emax model), and circadian night rhythm. In agitated infants, depth of sedation was best describe...
Neonatology, 2010
suggesting a better balance between oxygen delivery and demand. PNA ^ 10 days, comedication and absence of cardiopathy were associated with more subtle decreases in cerebral oxygenation and faster recovery. Conclusions: Propofol-induced decrease in HR, SaO 2 and cerebral oxygenation is short lasting while a decrease in MABP is observed up to 60 min. The variability in the effects of propofol is influenced by PNA, comedication or cardiopathy. Near-infrared spectroscopy can be used to assess hemodynamic effects of hypnotics on the cerebral oxygenation.
2014
The practices of anaesthesiology and intensive therapy are difficult to imagine without sedation or general anaesthesia , regardless of whether the patient is a newborn, baby, child or adult. The relevant concerns for children are distinct from those for adults, primarily due to the effects of anatomical, physiological and pharmacokinetic-phar-macodynamic (PK/PD) differences, which become increasingly important in the brains of children as they develop. The process of central nervous system maturation in humans lasts for years, but its greatest activity (myelination and synaptogenesis) occurs during the fetal period and the first two years of life. Many experimental studies have demonstrated that exposure to anaesthetic drugs during this period can induce neurodegenerative changes in the central nervous systems of animals. The extrapolation of these results directly to humans must be performed with great caution, but anaesthesiologists around the world must begin to debate the safet...
Canadian Journal of Anesthesia/Journal canadien d'anesthésie, 2000
Purpose: Neurologic complications occur following cardiopulmonary bypass surgery. We conducted a randomized, controlled, single-blind study to determine the effect of propofol on the redox status of cytaa 3 , and to evaluate its potential for decreasing neurologic complications. Methods and Materials: Twenty-four children (median age: 3.3 yr; median weight:14.4 kg) scheduled for elective cardiopulmonary bypass surgery were assigned to either the experimental group (Group P, given sufficient propofol to eliminate brain electrical activity as measured on EEG (i.e. burst suppression)) or the control group (Group C, no propofol). Near infrared spectroscopy data were collected at one-second intervals throughout the surgical procedures. Pre-and postoperative neurologic examinations were completed by a physician blinded to the group to which the patient was assigned. Change in cytochrome aa 3 data at 10-min intervals (10, 20, 30, 40 min) following start of bypass were compared between groups by repeated measures analysis of variance. Results: The patterns of change in redox state of cytochrome were different between the two groups (P < 0.002). The pattern of change within Group P was similar to that in hypothermic patients in Group C. There were correlations between change in cytaa 3 redox status and temperature in the control subjects. There were no gross neurologic complications in either group. Conclusions: Propofol appears to stabilize the energy supply/demand equilibrium of the brain during cardiopulmonary bypass surgery and thus theoretically could reduce the incidence or severity of neurologic complications. 3 et la température chez les sujets témoins. Aucune complication neurologique importante n'est survenue dans un groupe ou l'autre. Conclusion : Le propofol semble maintenir l'équilibre entre l'offre et la demande d'énergie cérébrale pendant une intervention chirurgicale avec circulation extracorporelle. Il pourrait ainsi réduire, en théorie, l'incidence ou la sévérité des complications neurologiques.
Journal of Neuroscience Research, 2014
Previously we observed that prolonged exposure to propofol anesthesia causes caspase-3-and calpainmediated neuronal death in the developing brain. The present study examines the effects of propofol anesthesia on the expression of tumor necrosis factor-a (TNFa), pro-nerve growth factor (NGF), and their receptors in the cortex and the thalamus. We also investigated how propofol influences the expression of Akt and X-linked inhibitor of apoptosis (XIAP) expression, proteins that promote prosurvival pathways. Seven-day-old rats (P7) were exposed to propofol anesthesia lasting 2, 4, or 6 hr and killed 0, 4, 16, or 24 hr after anesthesia termination. The relative levels of mRNA and protein expression were estimated by RT-PCR and Western blot analysis, respectively. The treatments caused marked activation of TNFa and its receptor TNFR-1 and pro-NGF and p75 NTR receptor expression. In parallel with the induction of these prodeath signals, we established that propofol anesthesia promotes increased expression of the prosurvival molecules pAkt and XIAP during the 24-hr postanesthesia period. These results show that different brain structures respond to propofol anesthesia with a time-and duration of exposure-dependent increase in proapoptotic signaling and with concomitant increases in activities of prosurvival proteins. We hypothesized that the fine balance between these opposing processes sustains homeostasis in the immature rat brain and prevents unnecessary damage after exposure to an injurious stimulus. The existence of this highly regulated process provides a time frame for potential therapeutic intervention directed toward suppressing the deleterious component of propofol anesthesia. V C 2014 Wiley Periodicals, Inc.
BMC Anesthesiology, 2021
Background Exhaled propofol concentrations correlate with propofol concentrations in adult human blood and the brain tissue of rats, as well as with electroencephalography (EEG) based indices of anesthetic depth. The pharmacokinetics of propofol are however different in children compared to adults. The value of exhaled propofol measurements in pediatric anesthesia has not yet been investigated. Breathing system filters and breathing circuits can also interfere with the measurements. In this study, we investigated correlations between exhaled propofol (exP) concentrations and the Narkotrend Index (NI) as well as calculated propofol plasma concentrations. Methods A multi-capillary-column (MCC) combined with ion mobility spectrometry (IMS) was used to determine exP. Optimal positioning of breathing system filters (near-patient or patient-distant) and sample line (proximal or distal to filter) were investigated. Measurements were taken during induction (I), maintenance (M) and emergence...
Journal of Anesthesia & Clinical Research, 2012
Introduction: Propofol is a preferred agent in neurosurgical anesthesia because of its favorable effects on cerebral hemodynamics and excellent recovery profile. Butorphanol is a synthetic opioid which is 5-8 times more potent than morphine and is known to provide stable hemodynamics during various surgical procedures. Owing to its unfavorable effects on cerebral metabolism and hemodynamics nitrous oxide has a debatable role in neurosurgical anesthesia. But studies on exact dose requirement during propofol induction and maintenance anesthesia along with butorphanol with and without the use of N2O during craniotomies are lacking. So we aimed at studying the requirement of propofol (used along with butorphanol) with and without the use of nitrous oxide in intracranial surgeries using bispectral index (BIS) monitoring. Material and methods: Fifty ASA grade I/II patients (16-60 years) scheduled for elective intracranial surgeries (≤ 4 hour duration) were included and were randomly allocated into two groups, group P and PN. All received IV midazolam and butorphanol at a dose of 30 µg/kg each. Anesthesia was induced with propofol and maintained on propofol with oxygen in air (1:1 ratio) in group P and nitrous oxide in oxygen (2:1 ratio) in group PN patients. BIS score of ≤ 40 at the time of endotracheal intubation, 50-60 during maintenance and ≥ 70 at extubation was maintained. The overall and maintenance dose requirement of propofol and the recovery profile were studied. Results: The overall and maintenance propofol doses were significantly higher in group P than group PN (100.02 ± 20.28 µg/kg/min Vs 79.62 ± 13.13µg/ kg/min; p<0.001) and (90.82 ± 19.13 Vs 71.26 ± 11.78 µg/kg/min; p<0.001) respectively. The recovery profiles were identical between groups. Conclusion: When used along with butorphanol the overall and maintenance doses of propofol without the use of nitrous oxide are 100.02 ± 20.28 µg/ kg/min and 90.82 ± 19.13 µg/ kg/min respectively which is more (p<0.001) than the dose required in combination with nitrous oxide (79.62 ± 13.13 and 71.26 ± 11.78 µg/kg/min respectively). J o u rn al of A n e s th es ia & C li n ic a l Resea rc h
British Journal of Anaesthesia, 2003
Background. The induction characteristics of propofol 1% and 2% were compared in children undergoing ENT surgery, in a prospective, randomized, double-blind study. Methods. One hundred and eight children received propofol 1% (n=55) or 2% (n=53) for induction and maintenance of anaesthesia. For induction, propofol 4 mg kg ±1 was injected at a constant rate (1200 ml h ±1), supplemented with alfentanil. Intubating conditions without the use of a neuromuscular blocking agent were scored. Results. Pain on injection occurred in 9% and 21% of patients after propofol 1% and 2%, respectively (P=0.09). Loss of consciousness was more rapid with propofol 2% compared with propofol 1% (47 s vs 54 s; P=0.02). Spontaneous movements during induction occurred in 22% and 34% (P=0.18), and intubating conditions were satisfactory in 87% and 96% (P=0.19) of children receiving propofol 1% or 2%, respectively. There were no differences between the two groups in respect of haemodynamic changes or adverse events. Conclusions. For the end-points tested, propofol 1% and propofol 2% are similar for induction of anaesthesia in children undergoing minor ENT surgery.
Frontiers in Pediatrics, 2019
Aim of the study: In selected surgical neonates and infants, the rapidity of induction and intubation may represent an important factor for their safety. Propofol is an anesthetic characterized by a rapid onset and fast recovery time that may reduce time of anesthetic induction and improve post-anesthetic outcome. The aim of this study was to evaluate the safety and efficacy of anesthesia induction in full-term neonates and young infants after propofol bolus administration. Methods: A retrospective case-control study including infants below 6 months of age, undergoing general anesthesia between 2011 and 2013, was carried out. Patients that received intravenous propofol bolus to induce anesthesia were compared to patients who received inhaled sevoflurane. Time to reach successful orotracheal intubation (OTI) was measured in seconds. The quality of OTI was defined as "excellent," "good," and "poor," based on established classification and was reported. Hemodynamic parameters as systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse pressure (PP), heart rate (HR), and oxygen saturation (SaO2) were collected before OTI (t0), at OTI (t1), and at spontaneous breathing recovery (t2). Main adverse effects were recorded for both groups. Results are median (IQ range) or prevalence; p < 0.05 was considered significant. Results: 160 infants were enrolled in the study, 80 received propofol and 80 inhaled sevoflurane. Major surgery (involving organs in the thoracic, abdominal, or pelvic cavities) was performed in 64 and 54% of patients in the propofol and sevoflurane group, respectively (p = 0.07). Patients in the propofol group showed a shorter time for OTI [11.5 (4.0-65) vs. 360.0 (228.0-720.0) seconds, (p < 0.0001)]. No difference was found in the quality of OTI between the two groups. No significant complications were recorded in either group. Conclusions: Propofol is a safe and effective anesthetic in neonates and infants permitting rapid induction of anesthesia and rapid intubation, without negative impact on the quality of intubation and haemodynamic compromise.
BMC Anesthesiology, 2015
Background: The purpose of this randomised, single-centre study was to prospectively investigate the impact of anaesthetic techniques for craniotomy on the release of cytokines IL-6, IL-8, IL-10, and to determine whether intravenous anaesthesia compared to inhalational anaesthesia attenuates the inflammatory response. Methods: The study enroled 40 patients undergoing craniotomy, allocated into two equal groups to receive either sevoflurane (n = 20) or propofol (n = 20) in conjunction with remifentanil and rocuronium. The lungs were ventilated mechanically to maintain normocapnia. Remifentanil infusion was adjusted according to the degree of surgical manipulation and increased when mean arterial pressure and the heart rate increased by more than 30 % from baseline. The depth of anaesthesia was adjusted to maintain a bispectral index (BIS) of 40-60. Invasive haemodynamic monitoring was used. Serum levels of IL-6, IL-8 and IL-10 were measured before surgery and anaesthesia, during tumour removal, at the end of surgery, and at 24 and 48 h after surgery. Postoperative complications (pain, vomiting, changes in blood pressure, infection and pulmonary, cardiovascular and neurological events) were monitored during the first 15 days after surgery. Results: Compared with patients anaesthetised with sevoflurane, patients who received propofol had higher levels of IL-10 (p = 0.0001) and lower IL-6/IL-10 concentration ratio during and at the end of surgery (p = 0.0001). Both groups showed only a minor response of IL-8 during and at the end of the surgery (p = 0.57). Conclusions: Patients who received propofol had higher levels of IL-10 during surgery. Neither sevoflurane nor propofol had any significant impact on the occurrence of postoperative complications. Our findings should incite future studies to prove a potential medically important anti-inflammatory role of propofol in neuroanaesthesia. Clinical trial registration: Identified as NCT02229201 at www.clinicaltrials.gov
Anesthesiology, 2002
Background Propofol is a commonly used anesthetic induction agent in pediatric anesthesia that, until recently, was used with caution as an intravenous infusion agent for sedation in pediatric intensive care. Few data have described propofol kinetics in critically ill children. Methods Twenty-one critically ill ventilated children aged 1 week to 12 yr were sedated with 4-6 mg. kg(-1).h(-1) of 2% propofol for up to 28 h, combined with a constant morphine infusion. Whole blood concentration of propofol was measured at steady state and for 24 h after infusion using high-performance liquid chromatography. Results A propofol infusion rate of 4 mg. kg(-1).h(-1) achieved adequate sedation scores in 17 of 20 patients. In 2 patients the dose was reduced because of hypotension, and 1 patient was withdrawn from the study because of a increasing metabolic acidosis. Mixed-effects population models were fitted to the blood propofol concentration data. The pharmacokinetics were best described by a...
British Journal of Clinical Pharmacology, 2002
This paper describes the pharmacokinetics and effects of propofol in short-term sedated paediatric patients. Six mechanically ventilated children aged 1-5 years received a 6 h continuous infusion of propofol 6% at the rate of 2 or 3 mg kg-1 h-1 for sedation following cardiac surgery. A total of seven arterial blood samples was collected at various time points during and after the infusion in each patient. Pharmacokinetic modelling was performed using NONMEM. Effects were assessed on the basis of the Ramsay sedation score as well as a subjective sedation scale. The data were best described by a two-compartment pharmacokinetic model. In the model, body weight was a significant covariate for clearance. Pharmacokinetic parameters in the weight-proportional model were clearance (CL) = 35 ml kg-1 min-1, volume of central compartment (V1) = 12 l, intercompartmental clearance (Q) = 0.35 l min-1 and volume of peripheral compartment (V2) = 24 l. The interindividual variabilities for these parameters were 8%, &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;lt; 1%, 11% and 35%, respectively. Compared with the population pharmacokinetics in adults following cardiac surgery and when normalized for body weight, statistically significant differences were observed the parameters CL and V1 (35 vs 29 ml kg-1 min-1 and 0.78 vs 0.26 l kg-1P &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;lt; 0.05), whereas the values for Q and V2 were similar (23 vs 18 ml kg-1 min-1 and 1.6 vs 1.8 l kg-1, P &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;gt; 0.05). In children, the percentage of adequately sedated patients was similar compared with adults (50% vs 67%) despite considerably higher propofol concentrations (1.3 +/- 0.10 vs 0.51 +/- 0.035 mg l-1, mean +/- s.e. mean), suggesting a lower pharmacodynamic sensitivity to propofol in children. In children aged 1-5 years, a pharmacokinetic model for propofol was described using sparse data. In contrast to adults, body weight was a significant covariate for clearance in children. The model may serve as a useful basis to study the role of covariates in the pharmacokinetics and pharmacodynamics of propofol in paediatric patients of different ages.
Anesthesia & Analgesia, 2006
Propofol is commonly used for the sedation of critically ill patients undergoing mechanical ventilation. These patients may develop tolerance during long-term administration. Here, we describe the development of tolerance to propofol's sedative effect in rabbits during prolonged mechanical ventilation. Six healthy male New Zealand White rabbits were endotracheally intubated and received propofol by continuous IV infusion to maintain sedation for 48 h. The propofol infusion rate (IR) was adjusted to maintain the desired level of sedation. Assessments of the sedation level were made every 30 min or earlier if there were signs of awakening. Propofol concentrations were measured in arterial plasma after every other IR adjustment, provided there was an adequate level of sedation, using high performance liquid chromatography, and calculations of systemic clearance rates were made. The mortality rate was 100% with a survival period of 30.8 Ϯ 6.0 h (mean Ϯ sd). The course of IR adjustments followed a 5-phase pattern: 1) steady IR (mean Ϯ sd duration; 1.2 Ϯ 0.6 h), 2) increasing IR (9.4 Ϯ 5.5 h), 3) steady high-IR (2.3 Ϯ 1.2 h), 4) decreasing IR (13.7 Ϯ 1.9 h), and 5) steady low-IR (5.0 Ϯ 2.7 h). The course of propofol concentrations during the experiment in relation to propofol IR followed a 3-phase pattern: 1) steady concentration with increasing IRs (6.0 Ϯ 2.7 h), 2) increasing concentrations with increasing IR (5.8 Ϯ 2.5 h), and 3) increasing concentrations with decreasing IR (18.8 Ϯ 3.3 h). Propofol systemic clearance rates were progressively increased for 6.0 Ϯ 2.7 h and then gradually decreased for 24.6 Ϯ 4.7 h. In conclusion, all rabbits developed tolerance to propofol's sedative effect within the first hours of administration related to changes to the drug's metabolic clearance.
Anesthesia & Analgesia, 2007
The glutamate-nitric oxide-cyclic guanosine 3&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;#39;,5&amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;#39;-monophosphate (cGMP) pathway is potentially an effective target for general anesthetics. Plasma cGMP concentrations are reduced after an increase in predicted plasma propofol concentrations during sedation in healthy adult volunteers. We hypothesized that an increase in measured plasma propofol concentration leads to a reduction in plasma cGMP in anesthetized children. Eighteen healthy children aged 46.8 (+/-19.6) mo, requiring general anesthesia for lower body surgical procedures were enrolled. After inhaled induction, tracheal intubation and initiation of intermittent positive pressure ventilation, caudal epidural analgesia was performed. Anesthesia was maintained using a continuous propofol infusion adapted from a previously published regimen to achieve predicted propofol plasma concentration of 6, 3, and 1.5 microg/mL after 30, 50, and 70 min, respectively. Samples for propofol and cGMP plasma concentrations were collected and analyzed using high-performance liquid chromatography and an enzyme immunoassay system. The plasma cGMP concentrations varied significantly (median [range]) 19.2 [11.8-23.5], 21.3 [14.6-30.8], and 24.9 [15.7-37.8] nmol/L among each predicted plasma propofol concentration, P &amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;amp;lt; 0.0001. The correlation coefficient (r) was -0.62. This study demonstrates that an increase in plasma propofol concentration leads to a decrease in plasma cGMP in healthy children, and could serve as a biochemical marker for depth of propofol anesthesia in children.
Indian Journal of Anaesthesia, 2015
Evolution of anaesthesia has been largely helped by progress of evidence-based medicine. In spite of many advancements in anaesthesia techniques and availability of newer and safer drugs, much more needs to be explored scientifically for the development of anaesthesia. Over the last few years, the notion that the actions of the anaesthesiologist have only immediate or short-term consequences has largely been challenged. Evidences accumulated in the recent years have shown that anaesthesia exposure may have long-term consequences particularly in the extremes of ages. However, most of the studies conducted so far are in vitro or animal studies, the results of which have been extrapolated to humans. There have been confounding evidences linking anaesthesia exposure in the developing brain with poor neurocognitive outcome. The results of animal studies and human retrospective studies have raised concern over the potential detrimental effects of general anaesthetics on the developing brain. The purpose of this review is to highlight the long-term perils of anaesthesia in the very young and the potential of improving anaesthesia delivery with the novel molecular approaches.
Canadian Journal of Anaesthesia-journal Canadien D Anesthesie, 2005
Journal of Neurosurgical Anesthesiology, 2016
Background: During awake craniotomy, the patient’s language centers are identified by neurological testing requiring a fully awake and cooperative patient. Hence, anesthesia aims for an unconscious patient at the beginning and end of surgery but an awake and responsive patient in between. We investigated the plasma (C plasma) and effect-site (C effect-site) propofol concentration as well as the related Bispectral Index (BIS) required for intraoperative return of consciousness and begin of neurological testing. Materials and Methods: In 13 patients, arterial C plasma were measured by high-pressure liquid chromatography and C effect-site was estimated based on the Marsh and Schnider pharmacokinetic/dynamic (pk/pd) models. The BIS, C plasma and C effect-site were compared during the intraoperative awakening period at designated time points such as return of consciousness and start of the Boston Naming Test (neurological test). Results: Return of consciousness occurred at a BIS of 77±7 ...

Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
 Gustavo Fabregat
Gustavo Fabregat
